Abstract
Many community health plans believe AI integration is out of reach. But soon artificial intelligence will be critical for their survival.
As the well-resourced commercial plans continue competing with community health plans for state contracts as they come up for bid, the organizations without AI will be at a disadvantage. That means mission-oriented community health plans neglecting AI could start to suffer—along with the potential for impactful shifts in health equity, rural health, and social determinants of health (SDOH).
A common misconception held by those in the public sector is that AI takes too much effort to install, implement, and maintain. Many “AI tools” could be built with ease of use in mind but instead are designed for organizations with large and skilled data science teams- Goliath organizations with ample resources and funding. When placed in the community context with its unique populations, they lose their usefulness and cause more work.
AI That Plays to Your Strengths
An effective AI product is not supposed to break the bank, complicate operations, or add to any human workload. If it’s doing any of that, it’s probably not true AI (or at least the type of AI worth your time).
Simply put, AI is a way to answer precise questions precisely. It should make life easier. It should be flexible and tailored to your priorities and workflows. It should also amplify your existing resources.
Community health plans often focus on what they don’t have (money, time, state reporting flexibility, etc.) and forget that their community ties give them an edge. With a smaller, more local member base, they can take more precise action and see quicker results because communities already know and trust them. The problem is that they may lack the bandwidth to choose the right action in the first place.
Siftwell can help. We customize our AI models to your goals and resource limitations. Then we partner with you to ensure you’re getting the best results with the least amount of effort.
But what could that partnership actually look like?
AI Models to Inform Population Health Initiatives
Many health plans want to predict which members could develop more serious, higher cost conditions before they happen. With this kind of insight, organizations can optimize their operations, enhance their budget, and improve health outcomes.
The Problem With Traditional Analytics
A traditional population health analytics approach may have you spend months providing a company meticulously-formatted data to then generate a ranked list of 10,000 “high-risk,” “medium-risk,” and “low-risk” members. That’s after you have spent months talking with them about which of their 30+ different off-the-shelf models are right for you. Not only does the approach add upfront work and lack nuance, but it also leaves a plan to its own devices to:
- Understand the full context of the results
- Design a strategy
- Execute a set of initiatives
This “Population Health 1.0” also may not take into account how SDOH or other local factors influence the data.
As a plan, that means you’re paying low-to-mid six figures for an ambiguous solution that requires extra work when you’re already strapped for time and money. And if managing existing member demand wasn’t challenging enough, this approach uncovers more members for you to somehow act on.
Bandwidth aside, identifying “emerging-cost members” is time sensitive—the sooner you can ramp up initiatives, the more time you have to engage members in outcomes-improving programs.
The Siftwell Difference
Siftwell doesn’t require upfront data work, data post-processing, or anything discussed above to drive impact. Nor do we have 30+ products “on the shelf.” Rather, we build models for the endpoint(s) you specifically want. In late 2022, we used a client’s existing datasets (made and used for state reporting) to design custom predictive models that delivered insights within weeks, not months.
One of these (called the Siftwell Population Health model) identified nearly 4,000 members at high risk of increasing costs. It then grouped the 4,000 into 50+ Member Profiles, each one representing members who share similar clinical challenges and SDOHs.
With these distinct Member Profiles, Siftwell engaged the client to understand which cohorts were impactable based on the plan’s existing infrastructure, resources, and programs. We helped the client build a highly targeted population health strategy centered around the hidden rising risk members that they could actually move the needle on.
Dodging Bias to Understand “Henry”
“Henry” was one of the 50 profiles and represented 76 new members who each cost the plan around $145 since enrolling that year. Because of their limited claims volume and low baseline spend, Henry members may have been overlooked by other, more biased predictive models—namely, the ones that don’t factor in health inequity and barriers to care.
However, Siftwell predicted these members to experience up to 66.2x increase in medical costs in the next year—a massive increase.
How? Our model took into account the barriers each Henry faces:
- Aged 60-65, Henry is at higher risk of developing age-related health complications.
- Living in rural areas with poor plumbing, Henry has limited access to reliably clean water and sanitation.
- With low levels of computer ownership and technology adoption, Henry is more isolated from providers and health-related support.
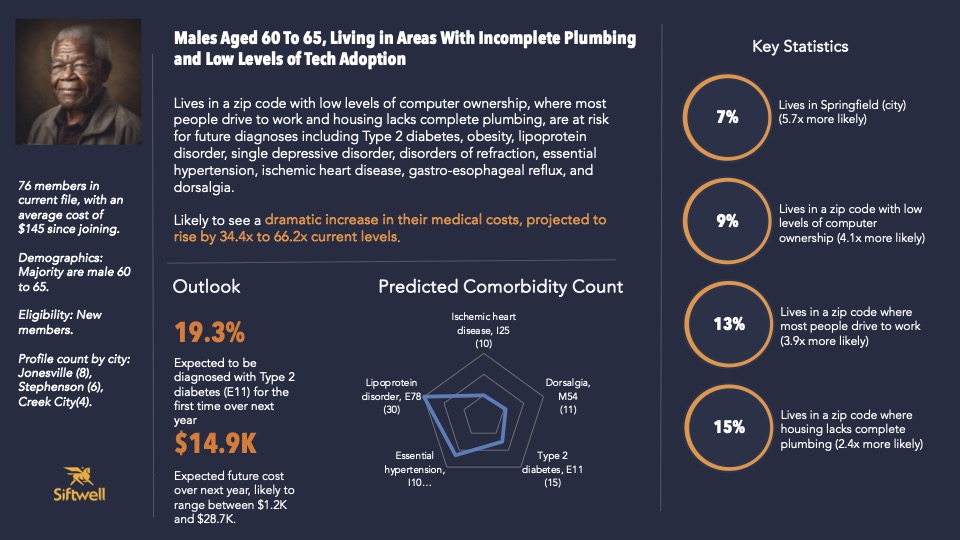
Then, from Henry’s existing clinical and claims data, we predicted that these members were more likely to be diagnosed with type-2 diabetes and lipoprotein disorders. If unmitigated, Henry’s emerging healthcare needs could cost the plan up to $28,700 per person per year.
The costs to each Henry’s life? Even greater.
With Great Precision Comes Great Impact
As your partner, we don’t just aim to predict the future. We want to help you change it, too.
The Member Profiles—rich with clinical, SDOH, demographic, and utilization-related context—allow you to understand your population in terms of cohorts of people, not health insurance claimants.
With this more holistic view, it’s easier to choose which “needle in the haystack” to move (there are often more than one). You can engage with those members with more precision and empathy. Then you can design human-centered initiatives that take advantage of existing or low-lift resources.
Moving the Needle for Henry
Henry is one such needle that our client may not have otherwise identified or had the ability to move. But because they better understood Henry’s story and circumstances, they were able to design a specific strategy around engaging Henry and getting “him” the right care for what “he” needs. These could look like:
- Implementing a rural health transportation program specific to his zip code(s) to help him get to his annual wellness visit.
- Calling him (rather than contacting him through a member portal or web application) and using a script tailored to his challenges.
- Offering him access to a virtual diabetes care program that allows him to receive care at home.
Depending on what you, and your health plan, has in place, each solution can be brought in and deployed specifically for Henry and others like him to maximize the impact of your outreach and intervention efforts. And because the initiatives are more targeted, they’re easier to accomplish and likely far more effective than the large-scale fixes of traditional or boilerplate models.
Siftwell Solutions Include Partnership
Henry is just one cohort of 50+ Member Profiles, so choosing what to do with each (and when to do it) may be overwhelming. But with a partner like Siftwell, it becomes easy. We help you prioritize and manage initiatives so you can focus on what you do best: serving your members.
Health Equity Initiatives As Compounding Investments
Micro-initiatives like these make members healthier, but they can also cause a ripple effect across the organization. The more effective and impactful a quality initiative is, the more likely it is to qualify for financial benefit or to help an organization hit its health equity goals. Healthier members are also shown to be more loyal. In fact, we have data suggesting that those who use fewer services are more likely to switch plans.
This means that a simple low-lift campaign can also promote quality activities and help maintain enrollment. Three birds, one AI-enabled stone.