Abstract
The CDC defines health equity as the state in which everyone has a fair and just opportunity to attain their highest level of health.
It is often spoken or written about as a future goal, not an integral part of what delivering healthcare means. We also rarely hear about what exactly is being done in the trenches to advance it or move toward it.
We know it’s important, so what can we do about it?
There’s no doubt that “health equity” is a high-priority topic these days for stakeholders across the healthcare ecosystem, from payors and providers to innovators seeking to apply AI responsibly across the healthcare spectrum. We won’t expound here on how these stakeholders are prioritizing health equity (see the ACO REACH program, which places specific emphasis on equity-related outcomes, for example) but it’s a topic we continue hearing about in boardrooms and at industry events. The 2023 AHIP Conference, for example, has at least 6 panels focused on health equity and there will no doubt be dozens more taking place through the balance of the year.
How do we make health equity a reality rather than an idea?
At Siftwell, we use data and AI to help our payor clients discover unfolding stories about their members so they can become more involved with them early on and champion equitable care. But AI can be a double-edged sword; if fed biased data, it can amplify health inequities. Foundational to our approach is building predictive models that account for systemic differences in healthcare utilization and cultural nuances. Whether it’s for population health initiatives (uncover emerging diagnoses, comorbidities, and high-utilization members), member retention and recruitment, or improving screening rates (for quality measures), we help payor executives and frontline teams understand:
- what specific member personas are in need and why
- what should be done for them
- who is most likely to engage
These are tricky questions that many operators today cannot answer. Answering them repeatably and empathetically to each member persona’s context, and then putting them into action, are what we live for at Siftwell. We call this identifying “actionable profiles.”
Let’s take a concrete example. A Siftwell client, a marketplace plan, sought to understand who within their membership was most at risk for developing costly comorbidities within the next year. The plan did not have the resources to contact and engage all their members to find the “needles in the haystack.” They lacked the analytics bandwidth to build, test, and refine their own predictive models. They also lacked the budget for a mid-six-figure “off-the-shelf” predictive analytics solution that would require strict templated data formats and 9-12 month timeframes to get off and running. There is much more cost here than the price tag, as most health plan executives would agree.
Siftwell started working with the client in late 2022 and custom-built several predictive models from datasets that they already had on hand, with no upfront data work needed and first insights coming in weeks rather than months. Among the models built was for predicting emerging diagnoses and comorbidities as well as emerging cost, or Siftwell’s Population Health model.
The Population Health model uncovered 50+ profiles for new members expected to see significant cost increases, representing nearly 4,000 members (or roughly the top 10% of membership). The 50 profiles each contain members who share certain demographic, geographic, clinical, or other characteristics that have predictive value. Not surprisingly, health equity-related and SDOH-related factors showed up repeatedly throughout the data and are some of the biggest predictors of outcomes.
Take the profile below, who we’ll call “Henry.”
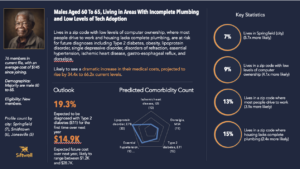
Henry is an actionable profile of 76 members, each of which are new members (they have less than 12 months of claims history) and have cost an average of $145 since joining the plan. They have low baseline spend, minimal claims volume, and other associated factors (more on those below) which make them susceptible to bias in predictive modeling. Based on Henry’s characteristics, however, Siftwell predicted this profile to experience a 34.4x to 66.2x increase in medical costs—a dramatic increase.
We know that the Henrys are aged 60-65, and among other characteristics live in areas with incomplete plumbing and with low level of computer ownership and technology adoption – all SDOH factors that negatively impact health equity. Our models factored their low claims volume into our models so as to avoid systemic bias in our predictions. From these data, as well as the clinical and claims data paired with them, we were able to reliably predict that these formerly $145 members were soon to cost as much as $28,700 with one of the key drivers being likelihood to be newly diagnosed with type-2 diabetes and lipoprotein disorders.
Henry is in a delicate situation and needs help. Many plans already have the resources or partnerships to provide this care if they only knew how to find them. Discovering these unfolding stories in the data can supercharge community health plans to sustainably get involved in member care and give all members a fair and just opportunity to attain their highest level of health. That’s how we make health equity a thread that runs through everything, not a focus area in isolation.


