Abstract
Siftwell Pegasus transforms quality performance for health plans across all lines of business – Medicare, Medicaid, Marketplace, and Commercial – by unifying data intelligence with predictive member targeting to identify the most impactable members, optimize resource allocation, and deliver measurable improvements in HEDIS scores and cost reduction.
Quality leaders are under intense pressure to deliver results across multiple fronts. You need to hit HEDIS targets, improve Stars ratings, and reduce avoidable costs, all while managing stretched operational teams and unpredictable member engagement.
The reality is stark: Chronic condition management and preventative care measures like CBP (Controlling High Blood Pressure), GSD (Glycemic Status for Diabetics), AWV (Annual Wellness Visit), and BCS (Breast Cancer Screening) are major cost drivers for your plan. Traditional outreach campaigns struggle with low outreach response rates, no-shows, operational bottlenecks, and mysterious drop-offs that are nearly impossible to diagnose. You’re left wondering why members aren’t completing their annual wellness visits or why your team’s call-to-appointment conversion rates vary so dramatically.
Without clear visibility into these gaps and insight into how to optimize the resources you have, you’re flying blind on initiatives that directly impact both your quality scores and your bottom line. You already know your HEDIS performance and who’s compliant. What you don’t know is WHY gaps exist and WHAT TO DO about them.
Siftwell Pegasus: Your Unified Quality Intelligence Platform
We work with Quality teams that have identified targets but are challenged to close the gap of how to reach targets.
Siftwell’s Pegasus platform was built by health plan operators like you to transform how community health plans approach quality improvement by unifying your eligibility claims and operational data with over 15,000 proprietary data points.
The Four-Quadrant Approach to Member Targeting
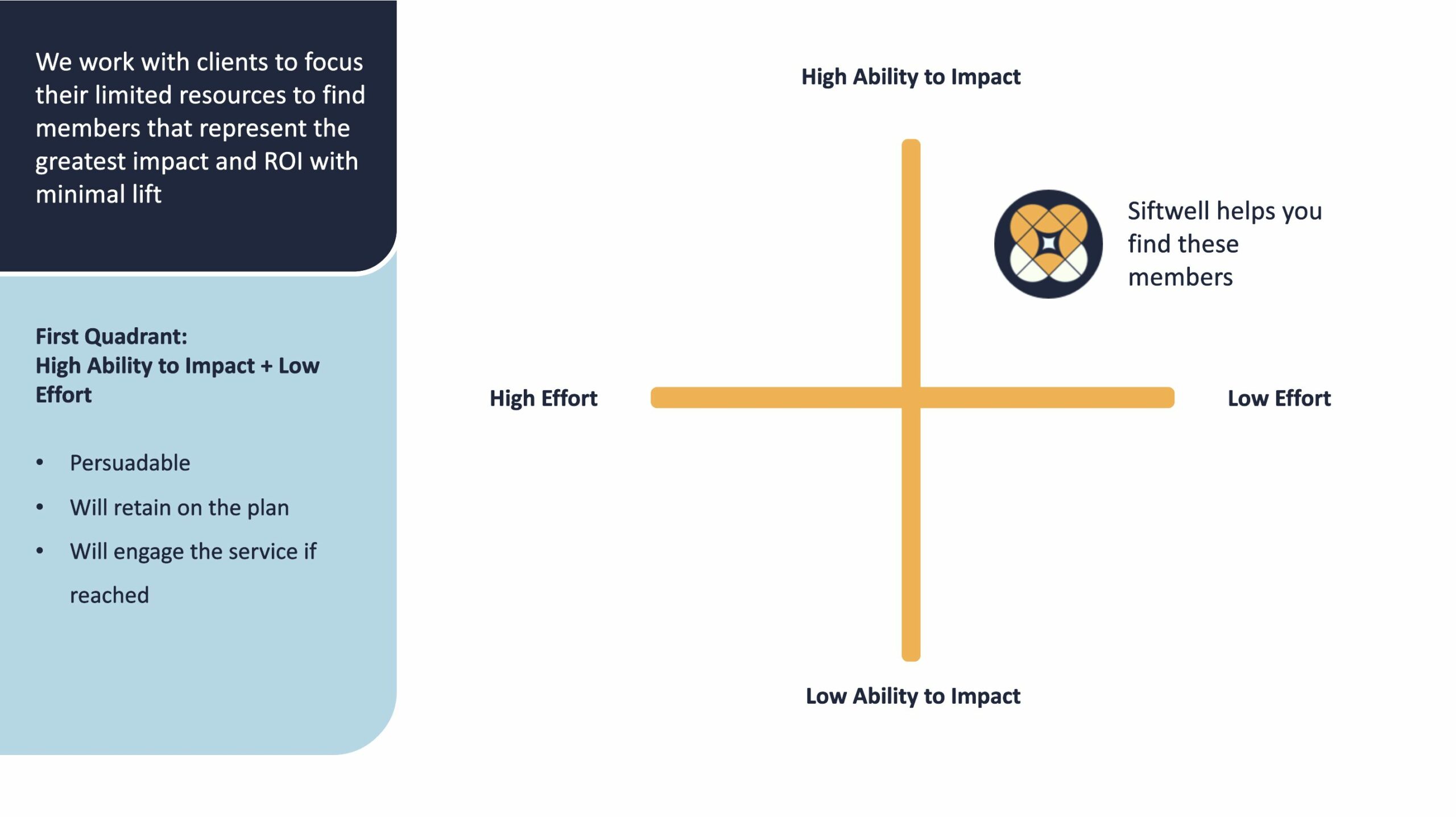
There are four distinct member groups:
- Low Ability to Impact + Low Effort: Limited quality impact; low ROI potential
- Low Ability to Impact + High Effort: Complex to engage; big lift for quality team
- High Ability + Low Effort: Sweet spot – quick wins with strong ROI
- High Ability + High Effort: High impact potential, but requires resource-intensive campaigns
Our clients focus their limited resources on the third quadrant: High Ability to Impact + Low Effort. These members represent the quick wins, where quality initiatives deliver the greatest impact and ROI with minimal lift.
However, Siftwell doesn’t ignore the other quadrants. Each requires different strategic interventions. The third quadrant represents the lowest hanging fruit for quick impact (that gets buy-in from your organization’s stakeholders), while other quadrants require longer-term intervention strategies tailored to their specific profiles.
By understanding which members fall into which quadrant, plans can deploy the right intervention at the right time, maximizing both short-term wins and long-term quality performance.
Target the Right Members at the Right Time
Machine learning models identify members most likely to close quality gaps, with predictive ROI modeling that shows expected outcomes before you launch campaigns.
Stop guessing. Start targeting with confidence.
Track Quality Measures That Matter
Monitor HEDIS improvement efforts across all chronic condition management (such as CBP, GSD, KED, EED, SPD) and preventative care measures (such as AWV, AAP, BCS, COL, AIS) in real time. Get instant visibility into target gaps and performance trends that cross Medicaid, Medicare, and Marketplace lines of business.
Operational Clarity Where You Need It Most
Campaign dashboards reveal exactly where member drop-offs occur and why. See if the issue is pickup rates, appointment scheduling, or attendance, then drill down to understand root causes like work schedule conflicts or childcare responsibilities.
Measurable Quality + Cost Impact
By improving chronic condition management and preventative care measures, Pegasus helps reduce unnecessary utilization while lifting your quality scores. Prevention and chronic condition management directly contribute to lower medical costs across your plan.
See Siftwell Pegasus in Action
Watch how community health plans use Pegasus to track, target, and close quality gaps, all in one place.
From unified data visualization to targeted member cohorts to campaign performance tracking, see how Siftwell Pegasus transforms quality initiatives from operational guesswork into data-driven success.
Key Benefits Summary:
- Predictive member targeting to determine persuadable, impactable member within high-priority care gaps, so effort is spent on those measures that will drive the biggest performance improvement
- Scenario modeling to determine greatest return on effort
- Operational Transparency that identifies drop-off points and reasons for noncompliance
- Cost Reduction through improved chronic condition management and preventative care
- Crossline Flexibility across all HEDIS measures and lines of business
Ready to Transform Your Quality Performance?
Stop struggling with disconnected data, unclear targeting, and operational blind spots.
Siftwell Pegasus unifies your quality initiatives with the intelligence and clarity you need to drive real results.
Prevention and chronic condition management are critical to controlling costs while improving member quality outcomes.
Let us show you how we can help your plan achieve both.
Testimonials
“[Siftwell] is not just a data company— you’re a healthcare company that uses data. That’s what makes this work… If you’re not using AI or something like this, you’re already behind. Just start.”
Blair Fjeseth
CEO, Mountain Health CO-OP
“Working with Siftwell showed us how AI isn’t just a buzzword— it’s a practical tool to decode patterns in utilization and guide our decision. It’s about actionable insights that actually help plans and their members.”
Erin Henderson Moore
CEO, Fidelis Care of NJ
“The Siftwell team has been instrumental in the next step, helping us prioritize the members who need us most through risk stratification and by identifying cohorts of members who would benefit the most from our services.”
Dr. LaDonna Battle
Chief Clinical Operations Officer, Trillium Health


